Your dentist can point you in the right direction for treatment for many different oral conditions, whether it is something treatable at our office or requires a specialist or referral to your primary care physician. Below, we look at some common oral health conditions, some of their underlying symptoms, and what treatment options are available.
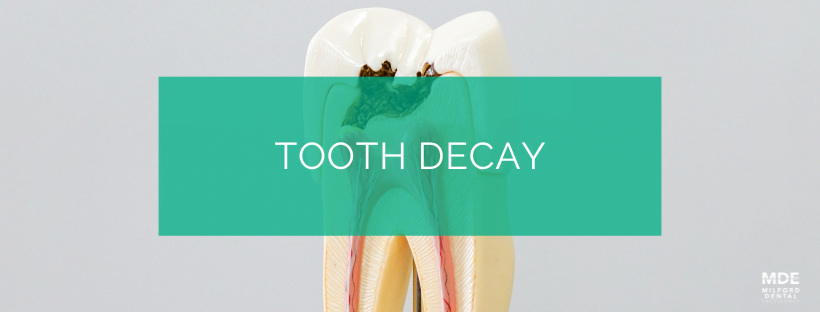
Tooth Decay
Tooth decay is a common degenerative oral health condition that results in the erosion of tooth enamel. The foods we eat contain sugars and starches. When combined with the bacteria that exists in our mouths, the result is plaque, a sticky substance that forms on teeth. Plaque produces acids that damage the surface of the teeth, resulting in holes that are called dental caries, or cavities. The National Institutes of Health reports that 92% of adults aged 20 to 64 have had at least one cavity.
Cavities
Cavities are holes in teeth resulting from tooth decay and can affect people of all ages. As they are most often tied to poor dental hygiene habits, they tend to be most common in children who are still learning the proper way to brush and floss. However, adults can get cavities as well. New cavities can form around the edges of areas of the tooth where previous cavities were filled in childhood, and receding gums from periodontal disease can expose lower portions of the teeth which do not have enamel and were previously protected from decay by the gums.
While tooth decay typically starts with the enamel of the tooth, it can affect all of the layers. The enamel is the hard outer surface of the tooth, followed by the dentin in the middle, and, lastly, the pulp, which contains the blood supply and nerve endings of the tooth. A cavity can take around three years to form in the enamel but will progress much faster through the softer inner layers of the tooth. Cavities do not cause any pain when they are in the enamel of the tooth, so without regular dental exams, it’s possible for them to go unnoticed until they have grown deeper and more severe.
Cavities are usually categorized by what part of the tooth they develop on and the extent of the decay. Cavity types include:
Smooth surface
These cavities form on the smooth surfaces of the teeth and are most often found in the spaces between teeth where toothbrushes have trouble reaching. Flossing and regular professional cleanings are the best way to prevent these from forming.
Pit and fissure
These cavities form on the tops of molars, in the crevices of chewing surfaces where food and plaque can be harder to remove. They tend to be more of a problem for people who don’t brush as often as they should, or those with poor brushing technique. Dental sealants are a good preventative measure against these types of cavities, as they can fill in the deeper areas and make it easier to keep the tops of the teeth clean.
Root decay
The hard enamel of teeth takes the longest to be affected by dental decay, but as we grow older, we are more susceptible to periodontal disease and gum recession. This exposes the softer dentin layer that was previously protected beneath the gum line. Root cavities are the result of tooth decay forming on these portions of the tooth.
Symptoms of Tooth Decay
Some of the common symptoms of tooth decay include:
- Bad breath
- Bad taste in the mouth
- Bleeding gums
- Toothache/oral pain
- Pain when biting down
- Sensitivity to hot or cold
- Sensitivity to sweet foods or drinks
- Tooth discoloration
- Visible holes or pits in teeth
Treatment of Tooth Decay
How tooth decay is treated depends on the severity of the decay.
Sealants
Useful in preventing cavities from forming in areas that you may find yourself having trouble keeping clean, sealants cover the surface of molars with a plastic material that fills in pits and crevices where toothbrushes may struggle to reach.
Fluoride
If tooth decay is caught early enough, fluoride treatments can be used to help remineralize the tooth enamel. You may also be asked to use a prescription toothpaste or mouthwash that will help to restore the minerals that acid has removed from your tooth enamel.
Fillings
When cavities have caused damage to the tooth enamel, it’s important to have the decayed portion of the tooth removed to halt any further progress of the cavity. The removed portion of the enamel can then be repaired with a dental filling.
Crowns
In cases where a large portion of a tooth has been affected by decay, the structure of the tooth may be weakened to a point where a filling alone would leave the tooth vulnerable to cracks. In these instances, a crown can be used to cover and protect the tooth.
Root canal therapy
Sometimes, when tooth decay is not addressed soon enough, it can reach the inner parts of the tooth and cause pain and serious problems. Root canal therapy is a method for removing the infected pulp from the center of the tooth and replacing it with a rubber-like material that prevents bacteria from getting back in.
Extraction
For cases where a tooth can’t be saved through root canal therapy, you may require an extraction to remove the infected tooth. Depending on the location of the tooth, your dentist may recommend a restoration such as a dental implant or bridge to prevent the surrounding teeth from shifting due to the gap.

Cracked Tooth
A cracked or fractured tooth is a common problem. Teeth can crack due to biting on hard foods, as a result of teeth-grinding, and may even happen over time as a result of aging. The extent of these cracks can range from small and mostly harmless to cracks that can cause the entire tooth to split into two or more parts. In all cases, the crack should be examined as soon as possible by a dental professional in order to determine what form of treatment is required.
Cracks can happen in the crown of the tooth (the part that is above the gum line), or the root of the tooth (the part below the gum line). They can affect only one or all three of the layers of the tooth: enamel, dentin, and pulp. The teeth most likely to develop fractures are the front upper teeth, and the mandibular molars, which are teeth toward the back of your lower jaw. Cavities and/or injuries can increase the likeliness and extent of damage of a tooth fracture.
Symptoms of cracked teeth
While not every crack will result in pain or symptoms, some of the ones that do may result in:
- Pain while biting or chewing
- Toothache that comes and goes
- Sensitivity to temperature changes or sweet foods
- Swelling around the tooth
- Pain around the teeth and gums that is difficult to locate
Types and Treatment
Different types of cracks may require different treatments. This is due to the location and extent of the crack.
Craze Lines
These are very small cracks that do not go past the enamel of the tooth. They are very shallow and cause no pain. Craze lines are common in adults, and usually are no more than cosmetic concerns.
Fractured Cusp
The cusp is part of the chewing surface of the tooth. Cracks here can often happen on teeth that have a filling. Fortunately, these usually don’t damage the pulp of the tooth and aren’t painful. Dental bonding or a new filling can repair the damage, or a crown might be suggested to protect the tooth.
Cracked Tooth
Usually, when a dentist talks about a cracked tooth, they’re referring to a crack that extends vertically from the chewing surface of the crown down toward the root of the tooth. This type of crack is at risk of spreading if not treated early. If the pulp of the tooth is damaged by the crack, saving the tooth may require root canal therapy.
The important thing is addressing the crack before it reaches the root of the tooth. If the crack reaches the root, it may no longer be possible to save the tooth, and an extraction could be recommended.
Split Tooth
Often the result of a cracked tooth that has progressed, a split tooth happens with a fracture that breaks the tooth into distinct parts. The location of the split will determine what parts of the tooth, if any, can be saved. Root canal treatment can sometimes be enough to save part of the tooth.
Vertical Root Fracture
These cracks begin at the root of the tooth and begin spreading up toward the chewing surface. Because of their location, they can easily go unnoticed and may only be discovered when the surrounding tissue becomes infected. Extraction of the tooth is the likely course of treatment, though, in some cases, a portion of the tooth may be saved through root canal therapy.
 Tooth Abscess
Tooth Abscess
An abscess happens when a bacterial infection causes a pocket of pus to form around a tooth. Abscesses have a number of causes and can affect not just the tooth, but the surrounding tissue and bone as well. Abscesses may even affect adjacent teeth. The types of abscesses are determined by where they are located. The three most common are:
Periapical Abscess
An abscess located at the tip of the root of the tooth. These are often the result of bacteria entering the pulp of the tooth through a cavity or fracture.
Periodontal Abscess
An abscess in the gum tissue that supports the tooth. These often result from gum disease and can spread to the surrounding area.
Gingival Abscess
An abscess in the gum tissue. These usually do not affect the tooth directly.
It is very important that tooth infections are treated, as they can otherwise spread to the jawbone, tissues of the face and neck, and even to the heart and brain in rare cases.
Symptoms of Abscessed Teeth
Some symptoms of an abscess include:
- Throbbing pain near tooth or gums
- Pain that increases when you lie down
- Pain when eating
- Red, swollen gums
- Tooth sensitivity
- Discolored teeth
- Loose teeth
- Bad breath
- Bad taste in the mouth
- Swelling in the face
- Swollen lymph nodes in neck or jaw
- Fever
- Difficulty in swallowing or breathing
Treatment
Treatment is vital in order to eliminate the infection and prevent further health complications. Treatment methods include:
Draining the abscess
A small incision will be made to allow for the pus to be drained. Once completed, the area will be cleaned with a saline solution.
Root canal therapy
If the pulp of the tooth is infected, root canal therapy can be used to remove the infection. A crown will typically be used to protect the tooth after the procedure.
Tooth extraction
If the damage to the tooth is too significant, making saving it with root canal therapy impossible, an extraction may be performed, instead. The extraction will also allow the abscess to be drained.
Antibiotics
Depending on the extent of the infection, you may be prescribed antibiotics to help eliminate the remaining bacteria.
Bruised Tooth
What is a bruised tooth?
While most people are familiar with bruises, it may be strange to consider the idea that a tooth can be bruised. However, your teeth have connective tissues and ligaments that hold them in place and cushion them against the kinds of forces they are subjected to during regular use. On an occasion when a tooth has been put under too much pressure or has experienced trauma, these tissues can become damaged or inflamed. This is known as a bruised tooth or sprained tooth syndrome.
Much like a bodily bruise, a bruised tooth can happen from an injury. This can be the result of a sports injury, a blow to the mouth, or things like biting down on a hard object or tooth grinding. The surrounding connective tissue will attempt to absorb the impact, but the capillaries around the tooth will burst, leading to discoloration—much as with any other type of bruise. Some degree of pain in the area may result as well.
The discoloration of a bruised tooth is usually a shade that varies between pink and gray. This color may be an indicator of the amount of damage the tooth has sustained. The pink color typically indicates that the tooth is in a stage where it is attempting to protect the nerve, though it can also be a sign of problems with the root of the tooth, so it is not safe to make an assumption based on color alone. The gray shade is a more likely indicator that the pulp of the tooth is dying, and there is a risk of decay or infection.
In all cases, you should contact the dentist to have an examination.
Symptoms of a bruised tooth
The first symptom you may notice with a bruised or sprained tooth is a dull, achy pain in the general area, similar to a sprained ligament. Alternatively, the pain may be located specifically in the affected tooth, where it may be a sharper type of pain.
The tooth may become discolored—turning somewhere between pink and gray, as mentioned above—and the surrounding gums could become sensitive and inflamed.
It may be difficult to distinguish the pain of a bruised tooth from toothache resulting from infection or tooth decay, so we recommend having your tooth looked at by the dentist.
How is a bruised tooth treated?
Whenever a tooth is showing signs of trauma, it is best to make an appointment to have it examined. X-rays will likely be taken to assess damage that might not be visible, and your mouth will be checked for loose teeth, sensitivity, or hidden problems like an abscess. Treatment will vary depending on the diagnosis. In cases where the bruised tooth is the result of teeth grinding, it may be recommended that you wear a nightguard to protect your teeth and ligaments from further damage. Mouthguards for sports are always recommended to protect teeth.
In many other cases, recovery for a bruised tooth will simply come down to giving the tooth time to heal. Over-the-counter modifications such as acetaminophen or ibuprofen can help with the pain from inflammation, and you should avoid further strain on the area if at all possible. Make sure you follow the treatment plan provided by the dentist to make sure your recovery goes as smoothly as possible.

